Webinar summary presented by Professor Eugene McCloskey
This blog summarises a webinar recording targeting APAC healthcare professionals interested in fragility fracture prevention, available on the Asia Pacific Bone Academy Knowledge Centre portal.
The video features Professor of Adult Bone Diseases at the University of Sheffield, Eugene McCloskey, UK, addressing the need for individualised treatment choices, particularly in those at highest risk for fracture.
Prof McCloskey maintains that a clear description of a patient categorised as high or very high risk for fracture, is still yet to be adequately defined, and can vary from country to country. Classification of very high risk can result from the presence of a combination of risk factors, and consideration of the time dependency of a given risk factor, such as a recent fracture (imminent risk).
Currently, most osteoporosis and fracture management guidelines globally offer a list of treatment options available to this patient cohort. However, they do not offer a recommendation on treatment efficacy. Some guidelines do however, offer health economics-related recommendations.
According to Prof McCloskey, as clinicians, we want to ensure our patients are on the most effective treatment, to reduce the occurrence of future fractures, and to mitigate fracture risk, particularly for those at highest risk for fracture.
“Thankfully we have a large and increasing pool of highly effective treatment options for reducing fractures and decreasing future fracture risk,” explains Prof McCloskey.
There are two main categories of treatment options available – antiresorptive treatment, such as oral and intravenous bisphosphates, and anabolic treatments, including parathyroid hormone peptides and anti-sclerotin. The chosen treatment depends largely upon patient preference, although physicians will consider the following when selecting a suitable treatment option for their patient:
- Fracture risk / probability;
- Prescribing restrictions / reimbursement;
- Past experience; and
- Lack of direct head-to-head studies to prove superiority of treatment options
(until recently).
In recent years, two substantial, and robust comparative studies in patients at the more ‘severe risk’ end of the fracture spectrum, were performed.
The first study published in The Lancet, in 2017, titled ‘Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial’ compared the anti-fracture efficacy of teriparatide with risedronate in patients with severe osteoporosis. This study found that among post-menopausal women with severe osteoporosis, the risk of new vertebral and clinical fractures is significantly lower in patients receiving teriparatide, than in those receiving risedronate.
Similarly, a second (ARCH) study published the same year (2017) in the New England Journal of Medicine (NEJM), titled ‘Romosozumab or Alendronate for Fracture Prevention in Women with Osteoporosis’, demonstrated that for postmenopausal women with osteoporosis who were at high risk for fracture, romosozumab treatment for 12 months followed by alendronate resulted in a significantly lower risk for fracture, than alendronate alone.
These two studies confirmed that anabolic treatments are far more effective in treating patients at high risk for fracture. The ARCH study further demonstrated significant benefit to this patient cohort commencing anabolic treatment, followed by resorptive treatment.
The availability of these more potent treatments is driving the need for personalised treatments on the basis of risk.
The webinar also showcases recent data obtained from an Icelandic cohort which examined the recency of fracture. This study identified a multiplier that can be applied to FRAX, to estimate an individual’s risk for future fracture, accounting for recency and the site of prior fracture, thereby generating superior predictive values.
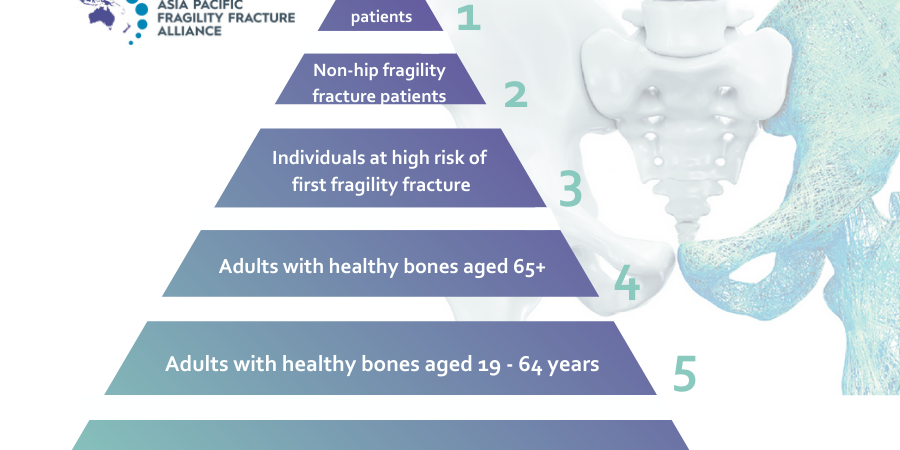
To gain access to many more informative resources, in addition to this webinar, please visit the APFFA Education Directory at https://apfracturealliance.org/education-directory/. The APFFA Education Directory is designed to connect patients, healthcare professionals, hospital administrators and policy makers in the Asia Pacific with relevant educational resources pertaining to best practice, to support optimal acute care, rehabilitation and secondary prevention of fragility fractures.