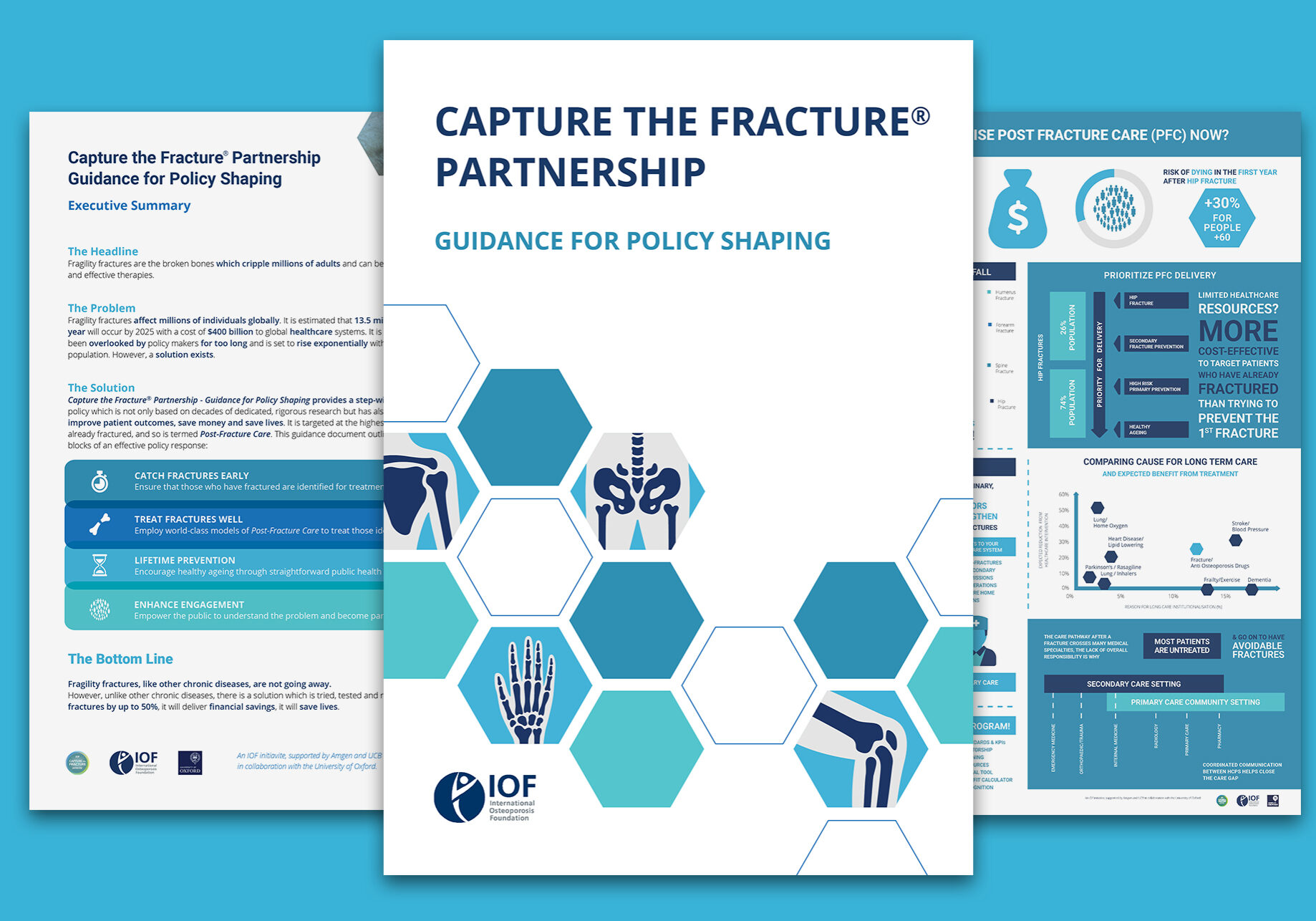
A new policy guidance published February 1, 2021, by the International Osteoporosis Foundation (IOF) – ‘Capture the Fracture® (CTF) Partnership – Guidance for Policy Shaping’ – highlights the urgent global need for Post-Fracture Care Coordination Programs.
The Guidance, issued under the framework of the Capture the Fracture® Partnership, sets out a step-by-step approach to building secondary fracture prevention policy, documented to improve patient outcomes, save healthcare costs, and save lives.1
Osteoporosis accounts for nearly nine million fractures each year worldwide,2 noting more than 200 million people are currently living with the devastating disease.3
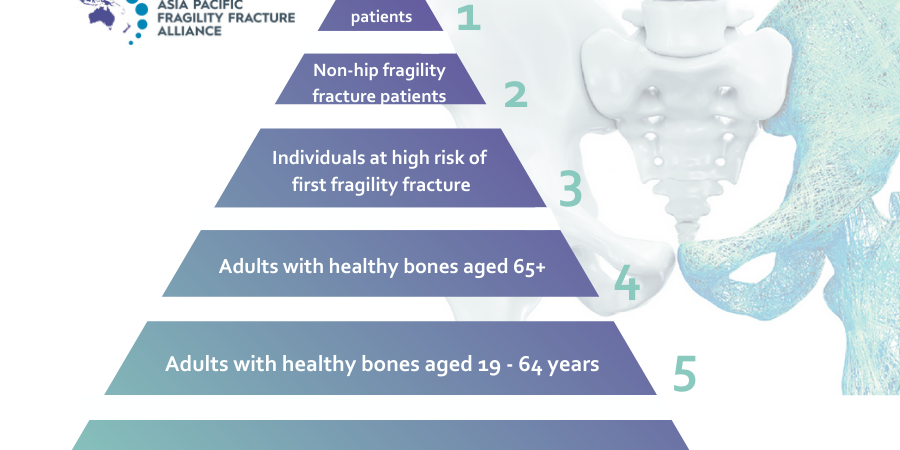
Despite the growing incidence of osteoporosis and subsequent fragility fractures worldwide, and the urgent need to prioritise fragility fracture prevention, up to 80 per cent of those who have already fractured a bone, are not being identified and treated with effective therapies.4 Concerningly, those who have sustained a first fragility fracture are five-times more likely to re-fracture.5
The Guidance offers a solution to the growing economic and health burden of the disease, advocates for a strategic approach to fracture prevention, and demonstrates the clear public health and financial benefits of Post-Fracture Care Coordination Programs, also known as Fracture Liaison Services (FLS). Wide-scale implementation of these effective programs serves to pave the way to addressing the fragility fracture crises compounded by our rapidly ageing global population.
In order to mount an effective global response to the growing burden of fragility fractures, health and social care services need to respond with robust identification and effective management of those at risk.
The four key simple building blocks proposed by the Guidance, for effective secondary fracture prevention policy include:
- Catch fractures early: ensure those who have sustained a fragility fracture are identified for treatment;
- Treat fractures well: employ world-class models of post-fracture care to treat those identified;
- Promote lifetime prevention: encourage healthy ageing through straightforward public health measures; and
- Enhance engagement: empower the public to understand the problem and become part of the solution.
According to IOF Chief Executive Officer, Dr Philippe Halbout, Switzerland, this new document confirms there is an overwhelming humanitarian and health economic case to be made for the implementation of secondary fracture prevention strategies, and specifically, Post-Fracture Coordination Programs. Osteoporotic fractures of the hip and spine in older adults are associated with increased risk of death and long-term disability, more frequent hospital admissions, and compromised independence, which impacts heavily on family carers, and frequently leads to nursing home admission.
“As the world’s largest organisation dedicated to bone health and osteoporosis prevention, IOF strongly urges the implementation of Post-Fracture Coordination Programs in all hospitals which treat fracture patients,” said Dr Halbout.
To learn more about the IOF’s ‘Capture the Fracture® (CTF) Partnership – Guidance for Policy Shaping’, head to IOF.
References
- Walters, S., et al., Fracture liaison services: improving outcomes for patients with osteoporosis. Clinical interventions in aging, 2017. 12: p. 117-127.
- National Institute for Health and Care Excellence. Osteoporosis assessing the risk of fragility fracture. [Jan, 2020]; Available from: https://www.nice.org.uk/guidance/cg146/resources/osteoporosis-assessing-the-risk-of-fragility-fracture-pdf-35109574194373
- International Osteoporosis Foundation (IOF). Osteoporosis Facts and Statistics. [Jan, 2020]; Available from: https://www.iofbonehealth.org/facts-and-statistics/calcium-studies-map.
- Royal Australian College of General Practitioners & Osteoporosis Australia, Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age. 2017.
- van Geel, T.A.C.M., et al., Clinical subsequent fractures cluster in time after first fractures. Annals of the Rheumatic Diseases, 2009. 68(1): p. 99-102.