The Asia Pacific Fragility Fracture Alliance (APFFA) has today (September 28, 2020) launched a comprehensive educational toolkit designed to arm primary care physicians (PCPs) with practical resources to aid the identification, assessment and ongoing management of those at risk of fractures, and thereby improve the safety and quality of patient care.
The APFFA PCP Education Toolkit contains a host of materials and templates to enable the planning and execution of two, one-hour-long, PCP workshops highlighting the growing burden of fractures, identifying patients at high risk of fracture, and reinforcing the importance of secondary fracture prevention.
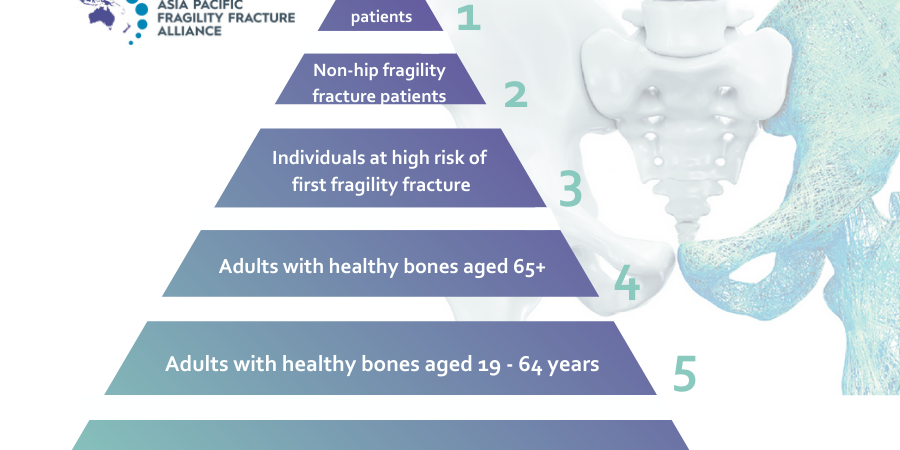
According to past President of the International Society of Clinical Densitometry and APFFA Education Working Group Chair, Professor Robert Blank, Sydney, the PCP Education Toolkit recognises the critical role PCPs can play in reducing the burden of osteoporotic fractures, which have devastating effects on survival, function and quality of life, by acting promptly and appropriately after the first fracture.1
“Due to the ubiquity of osteoporosis, PCPs are uniquely placed to identify and manage patients at risk of fractures. There are too many patients for all to be managed by specialists, even in well-resourced countries. Primary care therefore plays a critical role in preventing the health burden associated with osteoporosis, with the majority of medicines for osteoporosis initiated by PCPs.2,3
“While those who sustain a minimal trauma fracture may not always present to a hospital, almost all who do, will eventually see their PCP, positioning the PCP as pivotal to ensuring patients are appropriately managed post- fracture,”4 said Prof Blank.
“Currently, a concerning 70-85 per cent of patients presenting to their PCP or hospital with a minimal trauma fracture, are neither assessed for osteoporosis, nor appropriately managed, to prevent further fractures.”4
Osteoporosis accounts for nearly nine million fractures each year, worldwide,5 noting more than 200 million people are currently living with the disease.6 More than 1.1 million hip fractures were estimated to have occurred in China, Chinese Taipei, Hong Kong SAR, India, Japan, Malaysia, Singapore, South Korea and Thailand, respectively in 2018. By 2050, the number of hip fractures are projected to more than double, to exceed 2.5 million cases per annum.7
According to Orthopaedic Surgeon and APFFA co-Chair, Dato’ Dr. Joon-Kiong Lee, Malaysia, worldwide, older people represent the fastest growing age group, with the annual number of fractures likely to rise substantially with the ongoing ageing of this population. Even if age-adjusted incidence rates for hip fracture remain stable, the estimated number of hip fractures worldwide will rise from 1.7 million in 1990, to 6.3 million in 2050.8
“Disturbingly, despite the presence of generally safe and effective treatments, only a minority of low trauma fracture patients are evaluated and treated for underlying osteoporosis.9 In fact, the vast majority of older adults who sustain fractures do not receive subsequent interventions to identify and treat underlying, modifiable fracture risk factors,”10 Dr. Lee said.
According to Geriatrician and Gerontologist and APFFA co-Chair, Prof Derrick Chan, Taiwan, The PCP Toolkit materials emphasise how fractures in older adults compromise mobility, independence and quality of life. Furthermore, the Toolkit reinforces that the incidence of a fracture is sufficient to diagnose osteoporosis, regardless of a patient’s bone mineral density (BMD).1
“Less than a third of hip fracture patients regain their pre-fracture level of mobility,11 while more than 80 per cent are restricted with their daily activities, such as driving or grocery shopping.12
“Moreover, fractures beget fractures, with more than 30 per cent of all subsequent fractures occurring within the first year of one sustaining an initial fracture of the spine, shoulder or hip,”7 said Prof Chan.
Even with improvements in medical management, fracture patients continue to experience lower health-related quality of life. Those who have sustained fractures in more than one location, particularly of the spine, hip and upper leg, have a significantly compromised quality of life.”13
It is well established that a history of fracture is a strong predictor for future fractures. Following a fracture, a patient is five-times more likely to sustain another fracture within the first year.14 Spinal fractures, often the first fracture to be sustained by an osteoporotic patient, increase the risk of further fragility fractures, but are often clinically silent.4
“Some examples of practical tips available in the PCP Education Toolkit that can be used to bolster osteoporosis diagnoses in the primary care setting include identifying signs of vertebral fracture in older patients by documenting height loss, increases in thoracic spine kyphotic curve, unexplained episodes of back pain, and thoroughly assessing the spine on routine chest X-rays,”4 Prof Chan said.
The PCP Education Toolkit features recommendations to enable osteoporosis to be given more attention in clinical practice settings. Assets in the toolkit include a facilitator’s guide, workshop presentations and agendas, template invitations and promotional emails for distribution to prospective participants.
At the completion of each workshop, each participant will receive a certificate of completion courtesy of the APFFA Education Working Group.
“We encourage all PCPs to visit the APFFA website to download our comprehensive PCP Education Toolkit, in order to facilitate optimal fragility fracture management across Asia Pacific (APAC),” said Prof Blank.
Download the APFFA PCP Education Toolkit here.
To learn more, email secretariat@apfracturealliance.org.
References
- Conley, R.B., et al., Secondary Fracture Prevention: Consensus Clinical Recommendations from a Multistakeholder Coalition. Journal of Bone and Mineral Research, 2020. 35(1): p. 36-52.
- NPS MEDICINEWISE. Why osteoporosis matters. 2017 [Aug, 2020]; Available from: https://www.nps.org.au/news/why-osteoporosis-matters#r15.
- Australian Institute of Health and Welfare. Use of antiresorptive agents for osteoporosis management 2011 [Aug, 2020]; Available from: https://www.aihw.gov.au/getmedia/e4038a33-2c7f-431b-b4db-8468349eb364/11354.pdf.aspx?inline=true.
- Royal Australian College of General Practitioners & Osteoporosis Australia, Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age. 2017.
- National Institute for Health and Care Excellence. Osteoporosis assessing the risk of fragility fracture. [Jan, 2020]; Available from: https://www.nice.org.uk/guidance/cg146/resources/osteoporosis-assessing-the-risk-of-fragility-fracture-pdf-35109574194373
- International Osteoporosis Foundation (IOF). Osteoporosis Facts and Statistics. [Jan, 2020]; Available from: https://www.iofbonehealth.org/facts-and-statistics/calcium-studies-map.
- Ebeling, P., et al., Secondary prevention of fragility fractures in Asia Pacific: an educational initiative. Osteoporosis International, 2019.
- Sambrook, P. and C. Cooper, Osteoporosis. Lancet, 2006. 367(9527): p. 2010-8.
- Unnanuntana, A., et al., The assessment of fracture risk. The Journal of bone and joint surgery. American volume, 2010. 92(3): p. 743-753.
- David, M., HOW TO PREVENT THE SECOND FRACTURE: SYSTEMS FOR SECONDARY PREVENTION. Orthopaedic Proceedings, 2006. 88-B(SUPP_I): p. 11-11.
- Ebeling, P.R., et al., Building healthy bones throughout life: an evidence-informed strategy to prevent osteoporosis in Australia. Med J Aust, 2013. 199(S7): p. S1-s46.
- Cooper, C., The crippling consequences of fractures and their impact on quality of life. The American Journal of Medicine, 1997. 103(2): p. S12-S19.
- Adachi, J.D., et al., Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clin Proc, 2010. 85(9): p. 806-13.
- van Geel, T.A.C.M., et al., Clinical subsequent fractures cluster in time after first fractures. Annals of the Rheumatic Diseases, 2009. 68(1): p. 99-102.