Webinar presented by Professor Ding-Chen (Derrick) Chan, Taiwan
This blog summarises a webinar conducted by Professor Ding-Chen (Derrick) Chan, Vice Superintendent, National Taiwan University Hospital, Hsin-Chu Branch and Co-Chair, APFFA Joint Steering Committee, Taiwan, on the importance of taking a multidisciplinary, holistic approach to managing osteoporosis in older patients who present with multiple comorbidities.
The webinar recording is available on the Asia Pacific Bone Academy Knowledge Centre portal and can be accessed via the APFFA Education Directory.
Prof Chan commences the webinar by introducing a patient case study – an 87 year-old woman measuring 150 cm in height, 55.4 kg in weight, who has a BMI of 24.6 kg/m2. The woman has no prior history of smoking, alcohol use or betel nut chewing, and presented with a plethora of chronic illnesses including, but not limited to, hypertension, type II diabetes mellitus, osteoarthritis in the hip, gout and Parkinson’s disease.
Given the patient was previously treated by separate cardiology, neurology and urology clinics, she chose to visit a geriatric clinic to have one doctor as her point of contact, and to receive integrated care.
Prof Chan outlines the importance of geriatricians advocating for, and conducting a comprehensive geriatric assessment (CGA) – a multidimensional and interdisciplinary diagnostic process to identify the needs and plans of care, to improve the health outcomes of frail, older people. This assessment is performed by a multidisciplinary team of health professionals, including physicians, nurses, therapists and geriatricians.
“CGA evaluates the patient’s functional status, their physical and mental health, as well as socio-environmental factors.
“The main goal of CGA is to promote quality of life and functional independence, for frail, older adults,” said Prof Chan.
When considering the physical health component of a CGA, a patient’s previous medical history is taken into account, and the patient’s current medication is evaluated for relevance. The next step is to identify any new and untreated medical problems, noting the case study under examination also had compression fractures and osteoporosis.
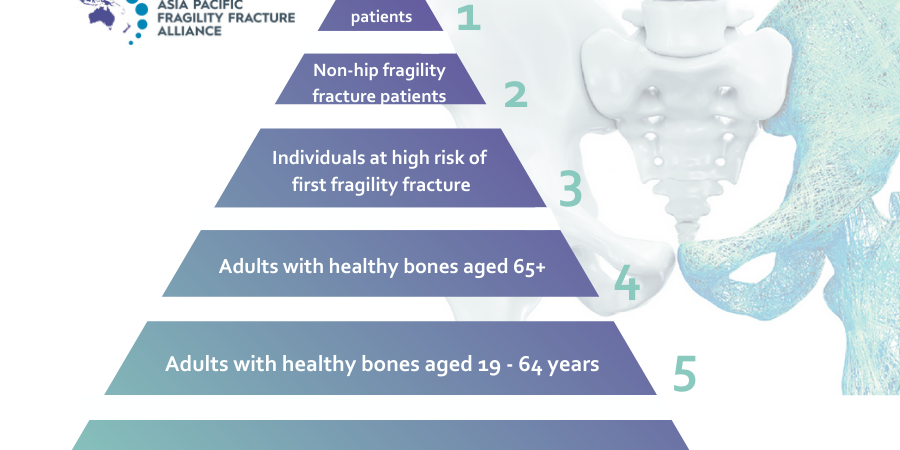
Prof Chan next provides an overview of the fracture liaison service (FLS) at the National Taiwan University, in which the patient case study was enrolled. Once enrolled in the FLS program, patients are assessed using tools such as FRAX®, bone mineral density (BMD) tests, and lifestyle risk assessments. If a patient has a hip fracture, they will also undergo a T/L spine X-ray, to identify any new compression fractures, and their falls risk will be evaluated.
“After assessing the patient, we determine which medication is best for them, and provide them with information and education via a care coordinator. We will also refer patients to any specialists they require, and regularly follow up with patients to check they are adhering to their medication,” Prof Chan said.
There are two ways to assess osteoporosis medication adherence – one indicator is ‘compliance’, and the other indicator is ‘persistence’. Compliant patients are defined as those with a medication possession ratio > 80 per cent (meaning they use more than 80 per cent of the medication they were prescribed). Patients considered to be persistent were those whose gap in prescription refills did not exceed 30 days.
“Research reveals the overall fracture risk reduction over a 14 year period in patients prescribed oral bisphosphonate is approximately 9 per cent among compliant patients, and 20 per cent among persistent patients.
“Adherence is usually increased when injection medication is prescribed, compared to oral medication,” said Prof Chan.
Referring once again to the case study, Prof Chan discusses the patient’s mental health (mild cognitive impairment and mild depression), and the impact of such on medication adherence.
“For the patient, family involvement is necessary to ensure high adherence to all medications.
“Given the patient had some mild cognitive impairment and mild depression, she initially lacked good adherence to alendronate (an oral medication), and was prescribed injection medications instead,” Prof Chan said.
“When the patient had a hip fracture episode, she had some delirium, which further impacted her medication adherence.”.
Prof Chan then investigates the patient’s functional status, in particular, her Barthel index score of 40/100, which means that she can barely ambulate with assistance. This makes it difficult for the patient to r regularly return to the clinic.
“Therefore, for this patient, six-month-to-one-year injections would be better for treating her osteoporosis to reduce the number of times she would be required to come to the clinic,” said Prof Chan.
Assessing the patient’s socio-economic status revealed that her daughter was her main caregiver and decision maker. The patient also had a foreign caregiver who lived with her, to help with physical tasks.
“Foreign caregivers are common in Taiwan. However, if you want the caregiver to give medication, you need to be very careful. Sometimes they do not give medication correctly. For example, the patient was originally taking alendronate once per week, so if she had accidently taken it once per day, then there would have been serious consequences,” Prof Chan said.
Prof Chan concluded by detailing the patient’s follow up data. Every six months a care coordinator would call the patient to arrange an appointment for her to receive her injection. Since switching to an injection, her medication adherence has neared 100 per cent. Furthermore, at the patient’s one year follow up, her calcium and Vitamin D intake had also improved.
In summary:
- When evaluating and managing older adults living with osteoporosis, it is imperative to take into account multiple co-morbidities (both physical and mental), functional status, and socio-economic conditions.
- Besides a standard osteoporosis assessment, a comprehensive geriatric assessment (CGA) should also be performed to address the above issues.
- Osteoporosis medication should be modified in response to changes in clinical conditions.
To gain access to many more informative resources, in addition to this webinar, please visit the APFFA Education Directory at https://apfracturealliance.org/education-directory/.