Patients living with osteoporosis are projected to increase in magnitude in the next decade. This means a crisis of bone fractures along with the forecasted increased societal and economic burden. Fortunately, substantial advances in the diagnosis and treatment of osteoporosis have emerged in the last decade.
In a new Therapeutic Advances in Musculoskeletal Disease review of scientific studies titled Osteoporosis in 10 years time: a glimpse into the future of osteoporosis, published on March 20, 2022, the authors focus on forecasts on the epidemiology of, and costs relating to osteoporosis in the next decade, and the future of osteoporosis diagnosis, fracture risk assessment, and treatment.1
The Scorecard for Osteoporosis in Europe (SCOPE) is an international project providing a comprehensive picture of total direct costs relating to osteoporosis care (fragility fracture treatment and pharmacological costs). The costs equate to an astonishing €37.4 billion or USD 41.03 billion in 2010, which increased to an even greater figure in 2019 to €56.9 billion or USD 62.43 billion (+64%). This observed increase was consistent with a 50 per cent increase in costs by 2025, proposed in 2007.2
More than 4 million fractures have been reported each year in Europe over the last 5 years. These numbers are projected to increase substantially in the next decade. In fact, the SCOPE analysis has estimated that the overall number of fractures will increase by a concerning 20 per cent by 2035.1Fortunately,effective interventions do exist, and this review outlines the following novel advances:
- Advances in imaging techniques
One of the most promising tools for estimating bone strength is the trabecular bone score (TBS). TBS can be easily implemented in most of the dual-energy X-ray absorptiometry DXA instruments.3 Hip-axis length is a way to measure the length from the great trochanter and the pelvic brim, and imaging processing software such as hip-strength analysis, and finite element analysis are other methodologies that, similarly to TBS, can be obtained from DXA analysis.
Radiofrequency echographic multi spectrometry is an innovative approach that uses ultrasound to analyse bone mineral density (BMD).4,5
Furthermore, high-resolution peripheral quantitative computed tomography is an alternative imaging technique that can provide both quantitative and qualitative information regarding the skeleton.
- Advances in biomarkers of osteoporosis
Micro RNA (miRNA) and long-non-coding RNA (lncRNA) are novel markers and targets of great interest in the field of osteoporosis.6 miRNA and lncRNA can control gene expression, and are widely recognised as crucial regulators of cell development and differentiation. Consequently, targeting miRNA-103a with antagomir-103a can rescue the osteoporosis caused by immobilisation and mechanical unloading.7
miRNA and lncRNA are versatile markers of disease and, more interestingly, they represent a novel therapeutic target. However, targeting miRNA and lncRNA is still a futuristic prospect, nonetheless, this field has expanded considerably, and the promise of having novel agents in the next decade is now realistic, according to this review.
- Mechanical testing of bone properties in humans might represent a novel approach for osteoporosis definition.8 As an example, external mechanical loading has been widely used in animal studies but some applications, such as dynamic hydraulic stimulation, might be envisioned for human applications too.9 In addition, magnetic resonance imaging may be considered in the future as it has been shown to effectively differentiate primary mineralisation defects (e.g. osteomalacia) from structure defects (e.g. osteoporosis), possibly allowing for new, cutting-edge, virtual biopsies.10
- Novel fracture assessment tools include machine learning and deep learning approaches that are rapidly revolutionising and improving our ability to predict health outcomes.11 The major advantages of the machine learning approaches over standard risk algorithms is that hundreds of clinical variables are considered, prediction of risk is automatised based on available data and, more importantly, this approach can be easily applied and automatised to hospitals that use electronic medical records, thereby reducing the burden on clinicians.
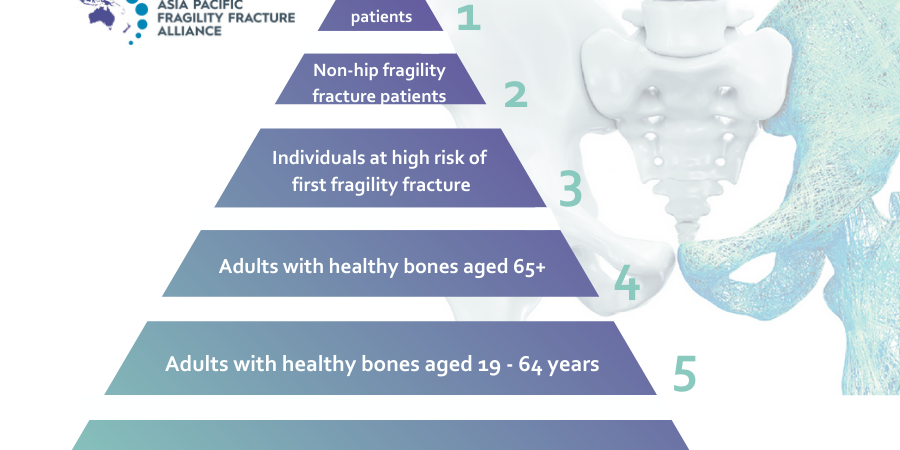
- Fracture liaison services (FLS) which involve the identification, investigation, and initiation of therapy, have been successful in reducing the incidence of new fractures.12 In the future, FLS harmonised across hospitals could leverage automated identification of individuals who fracture, and their subsequent referral to bone specialists. This in turn, will help to define the standard of care for FLS, and both refine and improve the health system intervention. Nevertheless, worldwide, there remains a lack of awareness for osteoporosis, and FLS is not yet routine clinical practice. The review’s authors, therefore, acknowledge that there is a long way to go to harmonising FLS.
- Anabolic agents as first line treatment are associated with a significant reduction of fracture risk, but their use is restricted to 2 years, and their discontinuation is associated with a decrease in BMD levels. Therefore, prompt treatment with antiresorptive after bone anabolic agents is encouraged.
To date, there are uncertainties regarding the most appropriate exit strategy following denosumab suspension. Pre-treatment with different antiresorptive drugs might yield different results. Nevertheless, combined treatment with bone forming and antiresorptive agents seems to be the best strategy in patients at high risk of fracture, according to the review’s authors.
Sclerostin inhibitors are now available for the treatment of osteoporosis and other metabolic bone diseases. Romosozumab, a sclerostin inhibitor, represents a new therapeutic option in the armamentarium of the bone specialists. Blosozumab is among the new sclerostin inhibitor in development, for which phase III study results are expected within the next few years.13 DKK-1 inhibitors are in development as well.14 The potentiality of dual inhibition (DKK-1 and sclerostin) is staggering. Dual inhibition was shown to enhance cortical bridging improving fracture repair to an extent that was not considered possible before.
Yet, despite these pharmacological therapies, treatment compliance is scarce. Therefore, complementary approaches are needed. Local osteo-enhancement procedure (LOEP) is an emerging surgical procedure that has been shown to effectively reduce the risk of re-fracture.15
In summary, while osteoporosis is projected to cause millions of deaths worldwide moving forward, the review’s authors maintain: “We can face this anticipated crisis with novel diagnostic, prognostic, and therapeutic strategies. In the next decade, we will have broader access to novel and more precise methods of fracture risk prediction. Patients at high risk of fracture will be more commonly referred to the bone specialist for treatment thanks to the diffusion of FLS. Osteoporosis treatment will evolve, we will have more confidence with combined and sequential strategies, and we will have access to novel and innovative pharmacological therapies.”
To read the full article click here.