Almost 40 per cent of individuals who experience a hip fracture are unable to walk, or will be institutionalised within a year post-fracture. Furthermore, 60 per cent require assistance one year later. Following a fracture, rehabilitation represents an integral component of the treatment pathway, and can improve a patient’s mobility, mortality and quality of life.
The Rehabilitation Working Group of the International Osteoporosis Foundation Committee of Scientific Advisors recently published a comprehensive narrative review in ‘Osteoporosis International’ exploring the global approach to rehabilitation post- fragility fracture. The review provides evidence for a range of rehabilitation strategies instrumental in the management of fragility fractures in patients without cognitive impairment, and further provides recommendations for future research.
The continuum of care for rehabilitation post- fragility fracture is highly complex, with improvements from rehabilitation, in some cases, realised nine and 12-months following fracture.
The narrative review delved into a plethora of scientific literature and clinical studies performed between 2010 and 2020. Key findings from the review include:
Exercise
- Multi-modal exercise post- fragility fracture to the spine and hip is strongly recommended to reduce pain, and improve both physical function and quality of life.
- Progressive resistance training, weight-bearing impact training, and functional balance, agility and coordination training should all be considered in managing patients at high risk of fragility fracture.
Physiotherapy
- Outpatient physiotherapy post- hip fracture has a stronger evidence base than outpatient physiotherapy post- vertebral fracture.
- Multi-disciplinary rehabilitation programs within the context of physiotherapy, may include behavioural interventions such as counselling, workbooks, goal setting, motivational interviewing and cognitive behavioural therapy. Research suggests psychologically-informed rehabilitation programs improve patient participation.
Nutrition
- Appropriate nutritional care, through dietary changes or supplements, after a fragility fracture provides a large range of improvement in morbidity, and reduces mortality.
- Some studies have also revealed that nutritional supplements may result in less medical complications (including fewer pressure ulcers and shorter wound healing times), fewer infections, reduced length of hospital stay, lower mortality, a preservation of BMD, and better muscle function.
Patient education
- Patient education not only heightens a patient’s understanding and knowledge of osteoporosis, but may also improve other health outcomes, such as health-related quality of life, physical activity, psychosocial functioning and adherence to both pharmacological and non-pharmacological treatments.
- Education may further improve other health outcomes, such as pain, and increase a patient’s ability to self-advocate.
- Despite being a useful tool in the management of osteoporosis, patient education has been highlighted as an area of unmet need among those living with osteoporosis and fragility fractures.
According to article co-author and Rehabilitation Working Group Co-chair, Assistant Professor Daniel Pinto, United States:
“Rehabilitation interventions result in considerable improvements for patients, and the benefits can be realised up to a year after fracture. However, rehabilitation modalities are both complex and inter-reliant, involving the interaction of exercise, nutrition, physiotherapy, falls prevention programs, and patient education, among other modalities.
“In this narrative review, we looked at distinct elements of a comprehensive approach to post-fracture management, and analysed the state of the evidence for each.
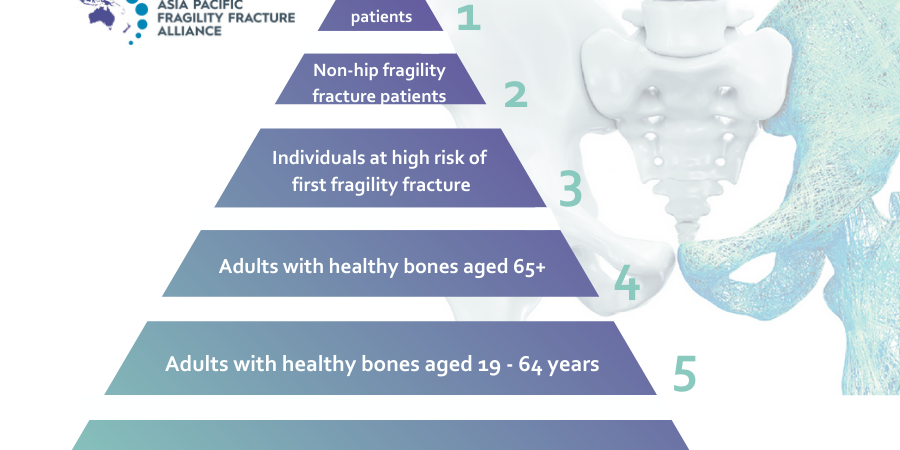
“The aim was to provide a succinct resource for clinicians and for Fracture Liaison Services (FLS), which are important providers of multidisciplinary post- fracture care,” said A/Prof Pinto.
The review concludes with recommendations involving areas that require further research, including the development of individualised exercise approaches considering patient preferences and factors designed to increase adherence; clinical trials to define the exercise regimens that may lead to the greatest reduction in kyphosis and pain after a vertebral fracture; clinical trials that define exercise regimens which ensure the best recovery and shortest length of stay in rehabilitation units; gaining a better understanding of the specific educational needs of patients and their carers; and trials on the implementation of rehabilitation strategies associated with FLS for secondary fracture prevention, among others.
To read the full article, click here.