There is a substantial gap in the care of osteoporosis and fragility fractures worldwide. To help address this gap, the International Osteoporosis Foundation (IOF) launched the ‘Capture the Fracture®’ program in 2012, to facilitate the implementation of Post-Fracture Care (PFC) Coordination Programs, such as Fracture Liaison Services (FLS), for secondary fracture prevention.
Despite the existence of such programs, evidence suggests fragility fracture programs alone are insufficient to close the osteoporosis care gap, given those with low bone mass but no history of a fracture, are not covered by FLS.
A recent study published in Osteoporosis International titled ‘One-year outcomes of an osteoporosis liaison services program initiated within a healthcare system’ evaluates the outcomes of an osteoporosis liaison service (OLS) delivered at the National Taiwan University Hospital (NTUH) within the main hospital (MH) and the Beihu branch (BB) over the course of a year.
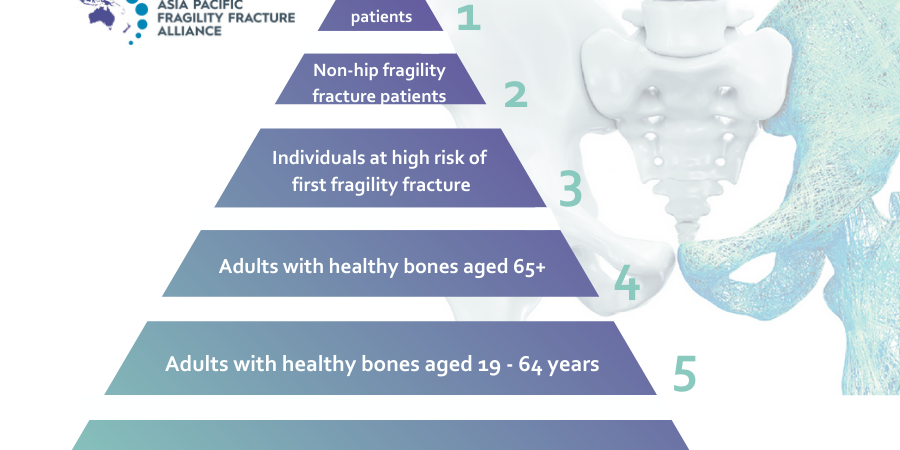
Similar to the Japanese program from 2011, OLS in Taiwan are coordinator-based programs providing comprehensive osteoporosis evaluation and care to enrolled patients through two complementary components – FLS and osteoporosis medication management services (MMS). In the study, MMS extended the osteoporosis care pyramid to those requiring osteoporosis care, who may be considered at high risk for fracture, but were unable to enrol in a FLS program due to their lack of fractures, or no new fractures.
The Taiwanese study enrolled 1,099 patients – 600 from the FLS program and 499 from the MMS program. Compliance with the IOF’s 13 Best Practice Framework (BPF) standards were evaluated and reported. These standards serve as a measurement tool for the IOF to award the ‘Capture the Fracture Best Practice Recognition’ to FLS, and although not all standards were completely applicable to all MMS study patients, they were applied as much as possible.
Key findings from the study include:
- Medication adherence rates reached more than 90 per cent at 12 months;
- Fall rates reduced from 47.7 per cent at baseline to 24.3 per cent at 12 months;
- Exercise rates improved from 57.6 per cent at baseline to 74.4 per cent at 12 months;
- Adequate protein intake increased from 74.3 per cent to 91.6 per cent at 12 months;
- Calcium supplementation rate improved from 57.5 per cent to 84 per cent at 12 months; and
- Vitamin D supplementation rate improved from 54.5 per cent to 80.9 per cent at 12 months.
The study also found the overall re-fracture rate (4.0 per cent) to be lower than that reported in the National Health Insurance data analysis (5.15 per cent), while one year mortality rates were also generally lower.
To achieve high medication study adherence rates, care coordinators were responsible for providing medicine-related education to patients, reminding physicians to order regular blood tests, and conducting regular patient telephone interviews. The study found that dedicated healthcare professionals (not necessarily nurses or pharmacists), coupled with well-designed protocols, are key to improving medication adherence.
According to study co-author and Co-Chair of the Asia Pacific Fragility Fracture Alliance (APFFA), Professor Derrick Chan, Taiwan, with the incidence of osteoporosis and its consequence, fragility fractures, on the rise in the Asia Pacific region, it is important to assess the effectiveness of OLS programs.
“Offering both FLS and MMS as complementary components of OLS improves care levels for more patients with osteoporosis, which ultimately helps us to close the osteoporosis care gap.
“To date, exponential increases in the numbers of FLS programs implemented worldwide have been recorded by the IOF’s Capture the Fracture® program, so a reasonable next step would be to promote osteoporosis care to other groups at high risk of fracture,” said Prof Chan.
“Results from our study suggest that MMS could be considered as the next level expansion of FLS that can be seamlessly applied, in conjunction with FLS programs.”