The second Fragility Fracture Network (FFN) Asia-Pacific Regional Expert Meeting, hosted by FFN Malaysia, was staged virtually on October 24-25, 2020. Consultant Orthopaedic Surgeon, FFN Malaysia President and APFFA Co-Chair, Dato’ Dr. Joon-Kiong Lee, Malaysia, opened the meeting by thanking participants in advance for their contribution and insights, and the FFN for the opportunity, guidance and support provided in hosting this important event.
“Over 3,000 registered participants engaged in three simultaneously conducted FFN Regional Expert Meetings, staged across Asia Pacific, Europe and Latin America. Physicians, geriatricians, orthopaedic surgeons and paramedics from a number of countries attended various pre-recorded plenary sessions, live break-out sessions and discussions, workshops, poster exhibitions and live networking sessions over the two-day-long event.
“It was a novel experience for all delegates, who enjoyed a comprehensive suite of meetings, delivered virtually, which upheld the standards of excellence traditionally offered in face-to-face meetings,” said Dr Lee.
More than 3,000 delegates registered for the three FFN meetings, and participated in the various interactive weekend sessions worldwide.
The first session on day one was aligned with clinical Pillar I of the FFN Global Call to Action (CtA) – namely acute multidisciplinary care for those who sustain a hip, clinical vertebral and other major fragility fracture. Topics canvassed included orthogeriatrics and perioperative care challenges of older individuals with fragility fractures.
According to Geriatrician, FFN President-Elect and APFFA Joint Steering Committee member, Dr Hannah Seymour, Australia, the Orthogeriatric approach can be adapted locally in different countries.
“The key attributes required for success include leadership, resilience, collaboration and maximal use of existing resources. Effective acute management of fragility fractures is a prerequisite for the other pillars, to enable early, unrestricted weight-bearing, and for patients to regain function,” Dr Seymour said.
The second session was aligned with Clinical Pillar II of the CtA – rehabilitation: ongoing post-acute care for people whose ability to function is impaired by hip and major fragility fractures. This session detailed evidence supporting early weight bearing in hip fracture recovery, and explored the associated advantages and disadvantages. Nutritional intervention for fragility fracture patients and the implementation of integrated rehabilitation management for the fragility fracture population was also presented.
The second meeting day commenced with an in-depth exploration of Pillar III – prompt implementation of secondary prevention measures immediately following the first fragility fracture, for both younger and older populations.
The session provided an overview of the clinical pathways available to hip fracture patients who have undergone surgery, followed by a presentation on key performance indicators (KPIs) for effective secondary fracture prevention. A discussion about, and demonstration of Fracture Liaison Services (FLS) databases – an effective method for evaluating and benchmarking secondary fracture prevention – ensued.
Pillar IV – calling for the assembly of multidisciplinary national alliances to advocate for policy change, supporting implementation of the first three pillars; was an integral component of the second day’s agenda. Sixteen national FFNs have been established worldwide to date, 10 of which have been formed in the Asia Pacific region. This session reinforced the importance of Pillar IV for facilitating achievement of the first three pillars, and further expanded upon the FFN’s regionalisation strategy, and the role of national FFNs in addressing the growing prevalence, and burden of, osteoporosis.
The FFN has also developed a Guide to the formation of national Fragility Fracture Networks. The purpose of this guide, and associated web-based resources, is to help turn the CtA into ‘Actual Action’, by offering support to countries currently lacking a national, multidisciplinary alliance.
A presentation showcasing the APFFA Hip Fracture Registry Toolbox, outlining the key steps for establishing and rolling out national hip fracture registries, also featured on the meeting agenda.
Presentations, plenaries, breakout sessions, symposia, and live panel Q&A sessions generated healthy discussion and debate about how to optimally drive positive change worldwide, and within local markets.
Coinciding with the regional meeting, the FFN officially launched two all-inclusive Toolkits – the FFN Clinical Toolkit and the FFN Policy Toolkit – both of which were created to complement the recently published second edition of the Orthogeriatrics – The Management of Older Patients with Fragility Fractures textbook. According to Chair of the FFN Communications Committee, Paul Mitchell, New Zealand, “hip fracture registries provide a mechanism to benchmark care against national clinical standards, and have been associated with significant improvements in processes of care and patient outcomes. Once completed, the comprehensive APFFA Hip Fracture Registry Toolbox will serve as an additional complementary asset to the two FFN Toolkits.”
The FFN Clinical Toolkit aims to support the practical implementation of Pillars I – III. This asset will serve as a valuable resource for members of the global and national FFNs, leaders and members of existing national multidisciplinary alliances, members of FFN sister organisations with a focus on geriatric medicine, orthopaedics, osteoporosis and bone metabolism, nursing, rehabilitation and rheumatology, and individual clinicians championing for the need for improved fragility fracture care within their workplace.
The various sections of the FFN Clinical Toolkit, dedicated to each of the three clinical pillars, feature a summary of clinical effectiveness, cost-effectiveness and organisation of (i) orthogeriatric services (ii) multidisciplinary rehabilitation, and (iii) Fracture Liaison Services (FLS). A map of the current pathways of care, and benchmarking of care through clinical guidelines, standards and registries, is described in each section. Given the substantial variability in the current provision of acute care, rehabilitation and secondary fracture prevention worldwide, a stepwise approach to implementation relevant to each clinical pillar, is proposed.
The FFN Policy Toolkit is suitable for anyone wishing to engage with policymakers in a bid to enhance fragility fracture care, particularly those in the earlier stages of their policy engagement journey. The Toolkit outlines key components of effective policy engagement gleaned from real-world insights and experiences of fragility fracture prevention and care advocates.
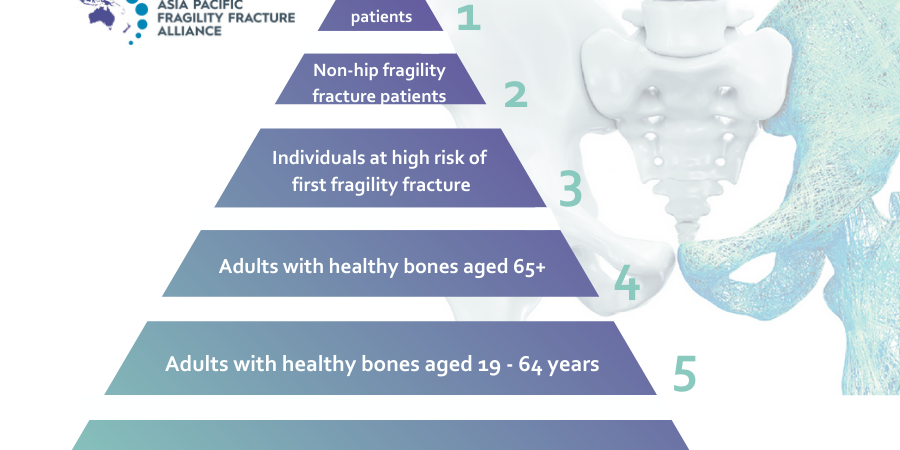
The FFN represents one of seven global and regional member organisations that constitute our organisation – the Asia Pacific Fragility Fracture Alliance (APFFA). Importantly, our mission at APFFA, is to promote multidisciplinary collaboration and change policy to facilitate best practice in the acute care, rehabilitation and secondary prevention of fragility fractures.