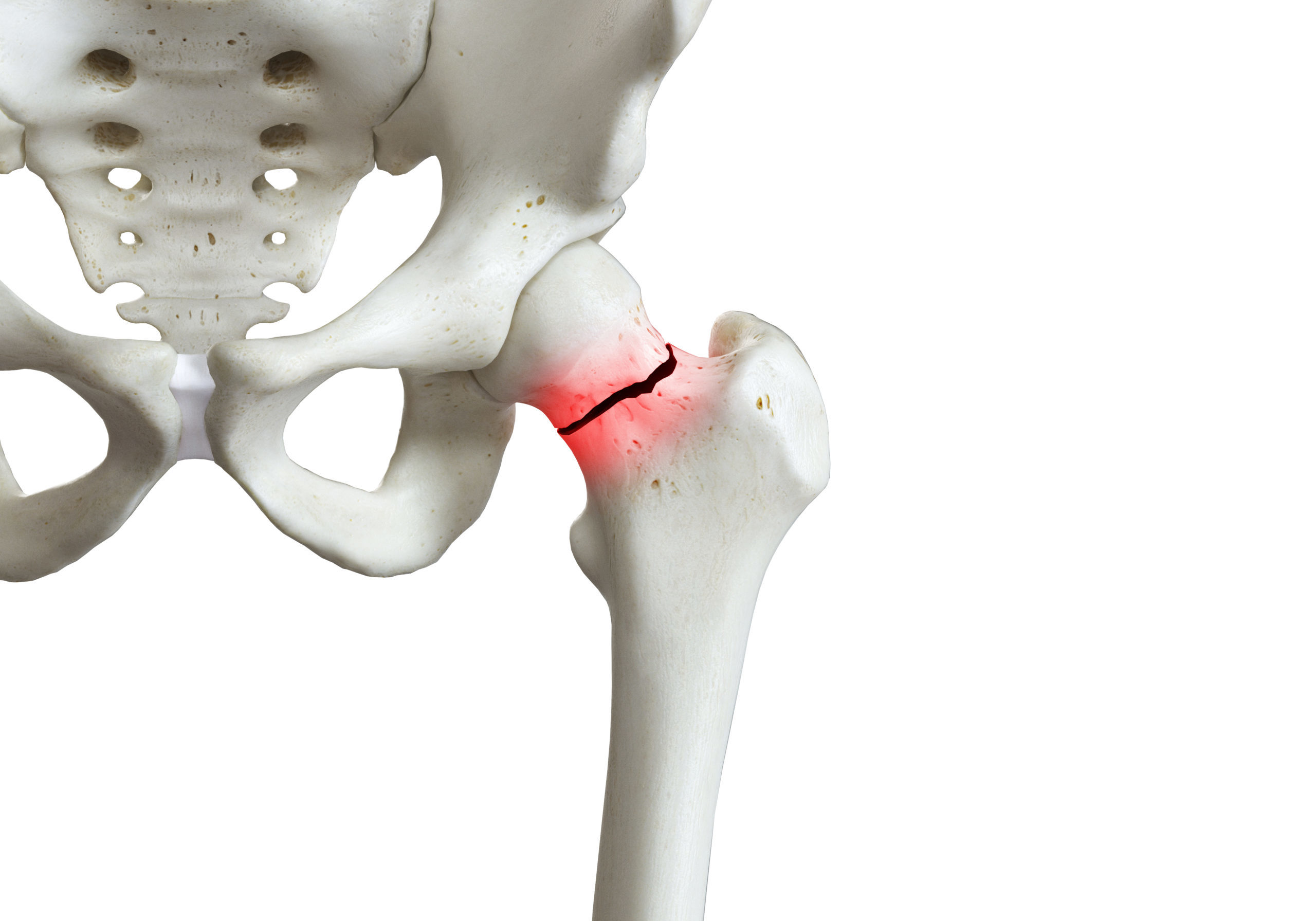
Hip or vertebral fractures in people aged 65 years or over is diagnostic of osteoporosis in the absence of another metabolic bone disease, regardless of bone mineral density, and is one of the strongest risk fractures for subsequent fractures. Fractures are not a normal manifestation of aging.
Osteoporosis is common. More than 1.1 million hip fractures were estimated to have occurred in China, Taiwan, Hong Kong SAR, India, Japan, Malaysia, Singapore, South Korea and Thailand alone, in 2018. Back, wrist, clavicle (collarbone) and pelvis are other common fracture sites.
Fractures threaten ambulation, independence and quality of life. In the case of hip fractures, only between one-third to a half of hip fracture survivors regain their ambulatory function.
Recent fracture is a powerful risk factor for subsequent fractures. Fortunately, fracture risk can be mitigated. The risk of sustaining a further fracture can be reduced by up to 30 to 40 per cent if the underlying osteoporosis and falls risk are managed by a secondary fracture prevention program.
Despite the substantive ability to reduce future fracture risk with treatment, osteoporosis-related fractures are under-treated. This is due in part, to misinformation about recommended approaches to patient care and discrepancies among treatment guidelines. Concerningly, only around one-in-five patients who have sustained a fragility fracture, have received medical attention.
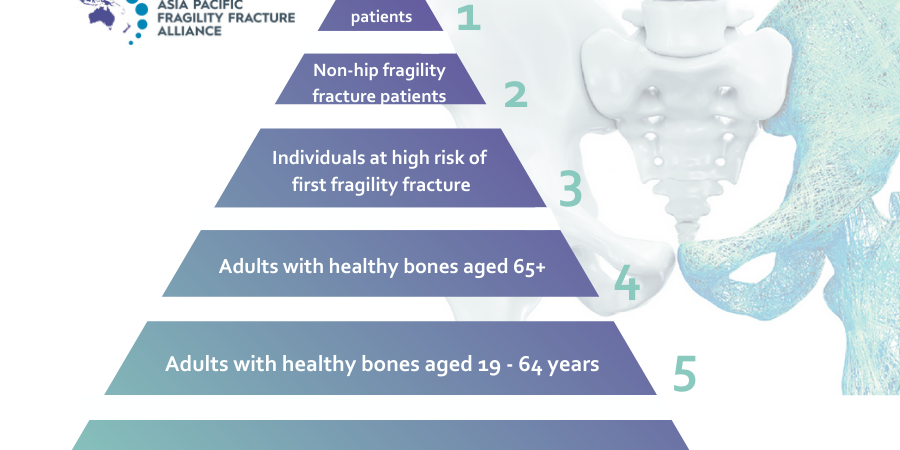
To address the under-treatment of osteoporosis-related fractures and heterogeneity in guidelines, the American Society for Bone and Mineral Research (ASBMR) assembled a multi-stakeholder coalition in 2017 to develop clinical recommendations for the optimal prevention of secondary fractures among those aged 65 years and older with a hip or vertebral fracture.
The 13 coalition-developed consensus recommendations published in the Journal of Bone and Mineral Research in 2019, address the gap that exists in the care of this patient cohort.
The recommendations are directed to all healthcare professionals involved in the care of these patients. The core fundamental recommendations emphasise the importance of:
- Communication – patients and their families must be made acutely aware that a broken bone is likely indicative of underlying osteoporosis, and places them at high risk of re-fracture, particularly in the 12-24 months following the initial fracture. It is also imperative to communicate that bone fractures often result in loss of independence and mobility, and an increased risk of morbidity. Most importantly, patients must be informed that appropriate action can be taken to reduce these risks.
- Awareness – a healthcare provider’s lack of awareness of their patient’s fracture history has been consistently identified as one of the key barriers to overcoming the provision of lifelong osteoporosis care.
- Regular falls risk assessments – the coalition’s recommendations call for a ‘history of falls’ record, evaluation of medications and comorbidities associated with increased fall risk and referral for complimentary therapies (physical, rehabilitative and psychiatric) to reduce the risk of falls. Up to one in six falls in older adults cause fractures, and around 90 per cent of hip fractures result from a simple fall from standing height or less, demonstrating falls prevention as a critical step in hip fracture prevention.
- Pharmacological intervention in a timely manner – given the risk of subsequent fracture is significantly elevated for patients at all levels of BMD, and that pharmacologic therapy for osteoporosis reduces the risk of fracture in older patients, treatment initiation should not be delayed.
- Supplementation – patients with osteoporosis are often vitamin D-deficient. Strong evidence indicates vitamin D reduces fractures when combined with calcium supplements in those at high risk of deficiency. Given calcium is critical for bone mineralisation and strength, dietary evaluation of the consumption of calcium is fundamental. Supplementation with vitamin D (800 IU per day) and calcium for those unable to achieve an intake of 1200 mg/d of calcium from food sources, is recommended.
- Routine follow up and re-evaluation – follow up and re-evaluation to reinforce patient education, monitor and evaluate the patient’s treatment plan, identify barriers to treatment adherence, and ensure regular falls risk assessments is recommended. Providing osteoporosis patients with the required educational support has proven pertinent in maintaining health-related quality of life. Conversely, failure to adequately meet a patients’ educational needs (e.g. medication, self-management, the nature of osteoporosis) has been shown to result in poor treatment adherence, and a decline in the doctor-patient relationship.
Additional recommendations include:
- considered referral to other appropriate HCPs;
- lifestyle modification (e.g. smoking cessation, less alcohol consumption, and emphasis on the importance of regular exercise); and
- discussion of the options, benefits, risks and duration of pharmacological interventions.
The recommendations emphasise that optimal management should occur within the context of a multi-disciplinary clinical system that includes case management, to ensure patients are appropriately evaluated and treated for osteoporosis and risk of further fractures.
Comprising seven global and regional member organisations from the geriatrics, orthopaedics, osteoporosis and rehabilitation sectors, APFFA embodies the coalition’s recommendations. The organisation aims to promote multidisciplinary collaboration, drive policy change and facilitate best practice in the acute care, rehabilitation and secondary prevention of fragility fractures, to ultimately deliver effective care, fewer fractures, and better outcomes for all people living in Asia Pacific.