Each year, more than 684,000 people die due to a fall worldwide, while another 172 million are left with short- or long-term disability. Moreover, 80 per cent of fall-related deaths occur in low- and middle-income countries, with regions of South-east Asia and the Western Pacific accounting for 60 per cent of these deaths.
Over the past two decades, fall-related deaths have risen faster than any type of injury, most likely due to rapidly ageing populations, increased urbanisation, and sedentary lifestyles.
To address this substantial and growing public health issue, the World Health Organization (WHO) published a comprehensive report titled ‘Step safely: strategies to prevent and manage falls across the life-course’ on April 27, 2021. This report is designed to support healthcare practitioners, policymakers, managers, researchers and advocates in their efforts to prevent falls, and to curb, and manage fall-related injuries. The report describes how falls are preventable, recommends fall prevention interventions based on current evidence, and describes how practical and policy interventions can prevent deaths and injuries throughout one’s lifetime.
In June 2016, the WHO Expert Consultation on Falls Prevention and Management committee met in Geneva to discuss an evidence-informed guide. The WHO subsequently commissioned researchers from the WHO Collaborating Centre for Injury Prevention and Trauma Care at The George Institute for Global Health, and the UNSW School of Population Health to conduct a review of high-quality global evidence on falls prevention, which later informed the ‘Step safely’ report.
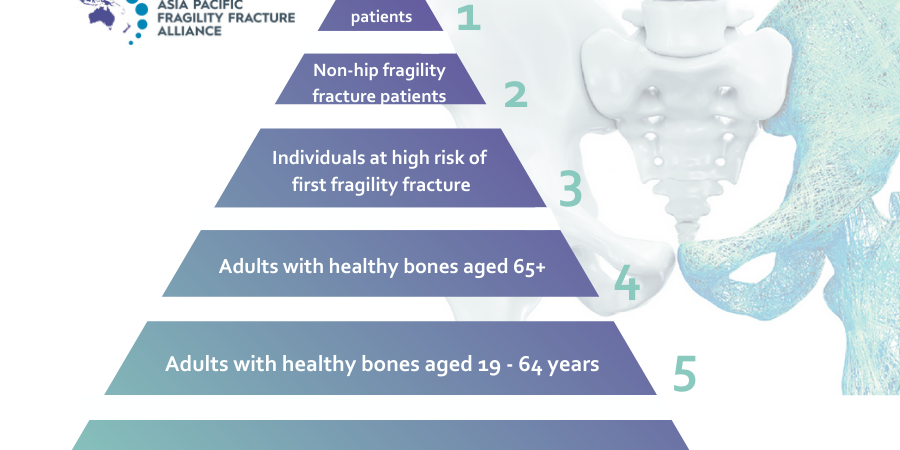
The WHO report focuses on the three specific population groups which account for the highest burden of falls and fall-related injury – older people, children and adolescents, and workers in high risk occupations. The report concludes with the following five overarching recommendations that aim to both prevent, and manage falls across these high risk groups:
- Encourage and enable physical activity throughout the lifetime to improve physical fitness, strength and balance for all. For children, this may include teaching them how to fall, in order to reduce injury, providing physical education within schools, and also sufficient opportunities for active play. For older people, exercise should focus on improving balance, function and strength, and bone density to prevent falls and their consequence, fractures.
- Create safe environments that encourage and enable physical activity. This includes reducing fall hazards in the home, providing soft-fall surfaces and safe equipment for children, installing barriers near fall hazards (including adequate scaffolding and guard rails on construction sites), and most importantly, educating the public on what they can modify in their own environments.
- Strengthen legislation and enforcement for example, in relation to construction safety, discouraging the use of baby walkers, and requiring landlords to install window guards in high-rise accommodation.
- Improve fall-injury data at global, national and local levels to enable monitoring and evaluation.
- Targeted programs for high-risk populations which, for older people, may include balance, gait and function exercises, home safety assessments, and medication reviews. For workers in high-risk occupations, this may involve the implementation of targeted workplace programs, such as ‘Slip, trip and falls’ (STF).
According to Steering Committee Member of the World Falls Guidelines, and Co-Chair of the APFFA Hip Fracture Registry Working Group, Professor Jacqueline Close, Australia, the use of certain medications and an inadequate diet can increase a person’s risk of falls.
“Although some medications can assist in the prevention of falls and fractures, such as medication for the treatment of osteoporosis, there are medications which can increase a person’s risk of falling.
These medications include those which have an impact on brain function, such as sedatives, antidepressants, antihypertensives and antipsychotics. As a result, these medications should only be used if absolutely indicated and should be prescribed at the lowest dose possible, for the shortest time possible,” said Prof Close.
“Older adults living in residential care often have low calcium and protein intakes, which can lead to weak bones and an increase in the risk of falls and fractures. A recent study from Australia found increasing intake of foods rich in calcium and protein, such as milk, yoghurt, and cheese, reduces falls and fractures in older adults living in residential care.”
Preventing falls can help achieve the United Nations Sustainable Development Goals linked to health and well-being, decent work, and safe, inclusive cities.
Crucially, we should no longer accept falls as inevitable accidents, or an inevitable part of ageing.
For more information, download the full report here: https://www.who.int/teams/social-determinants-of-health/safety-and-mobility/step-safely
To gain access to many more informative resources, in addition to the WHO Step safely technical report, please visit the APFFA Education Directory at apfracturealliance.org/education-directory.