A fragility fracture at any site is associated with reduced survival of up to six years, with the greatest reduction occurring within the first-year post- fracture, for those aged 65 years and over, according to a recent, real-world matched cohort study published in BMC Musculoskeletal Disorder.
This large, population-based, retrospective study compared 101,773 (74,557 female and 27,216 male) Ontario residents who had sustained an index fracture at any osteoporotic fracture site, with a matched cohort of non-fracture controls, to assess mortality risk post- fracture.
The Ontario study builds upon many studies spanning three decades from different countries and healthcare systems, that demonstrated a greater risk of mortality within the first year following a fragility fracture.
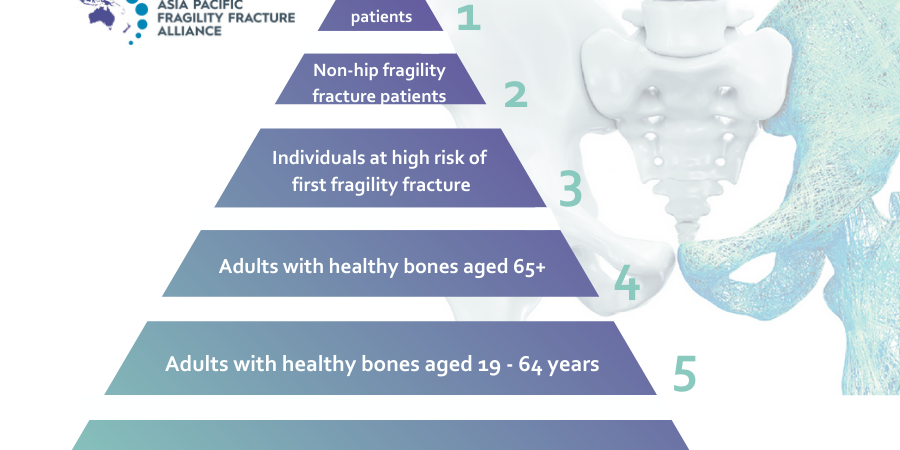
Despite the recognised mortality burden, studies confirm a large gap in the primary prevention of fracture, with an estimated 80–90 percent of adults not receiving appropriate osteoporosis management. The gravity of these facts is further amplified when considering that 90 per cent of patients with cardiovascular disease (CVD) are provided with appropriate, secondary preventative care.
According to Geriatrician, APPFA Joint Steering Committee member and FFN President-Elect,
Dr Hannah Seymour, Australia, studies examining post-fracture mortality following a non-hip fracture have typically focused on younger patient cohorts (aged ≥ 50 years), while studies examining mortality risk in adults aged >65 have predominantly assessed hip fractures patients.
“This 2021 retrospective matched cohort study of older adults aims to address a gap in understanding of the mortality risks associated with non-hip osteoporotic fractures in adults aged over 65.
“Addressing the fracture prevention gap is substantially more important for people aged over 65. Skeletal fragility in combination with a greater propensity for falls as we age combine together to increase fractures,” said Dr Seymour.
“This study revealed a fragility fracture at any site is associated with a doubling of mortality risk.
Significantly, a year post- fracture, absolute fracture risk was 12.5 per cent in women with a history of a fracture, and 19.5 per cent in men, compared to only 7.4 per cent and 13.4 per cent respectively, in the matched non-fracture controls.
“Further analysis of the data revealed that within the first year following a non-hip fracture, risk of death was in 1 in 11 women and 1 in 7 men. This study confirmed the high rate of mortality after a hip fracture as 1 in 5 women and 1 in 3 men die in the year following a hip fracture,” Dr Seymour said.
This study fuels the argument for a more proactive and preventative approach to osteoporosis management.
Healthcare initiatives have been implemented to address the care gap, and have certainly demonstrated efficacy in reducing subsequent fracture and mortality. Such initiatives include the orthogeriatric care model and fracture liaison services (FLS). Intervention can reduce the risk of future fractures between 20 and 50 per cent, and FLSs have been shown to deliver significant financial savings, and reduce mortality.
APFFA, together with other international and regional organisations, is calling for increased awareness and policy change to facilitate optimal fragility fracture management across the
Asia Pacific region.