Taiwan’s society is ageing rapidly. By 2026, it is projected that Taiwan will become a super aged society – when the proportion of a society’s population aged 65 years and older exceeds 20 per cent.
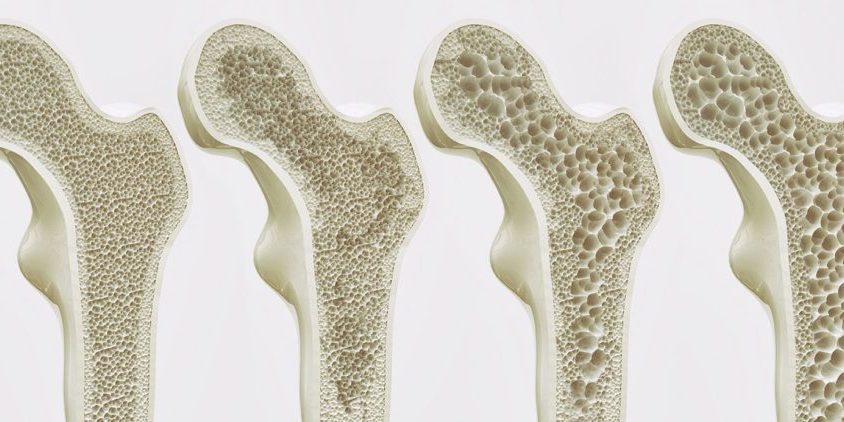
Osteoporotic hip fractures are a serious issue among elderly Taiwanese. Those who survive a hip fracture often experience decreased morbidity, lower quality of life, greater dependence on family, and increased medical requirements. Tragically, only 30 to 40 per cent of hip fracture patient’s return to their prior level of function.
A national Taiwanese population study published in Bone in September 2021, titled ‘Treatment of osteoporosis after hip fracture is associated with lower all-cause mortality: A nationwide population study’, strove to determine whether anti-osteoporosis treatment may reduce overall mortality after hip fracture surgery. Researchers utilised the extensive National Health Insurance Research Database (NHIRD) of Taiwan to identify patients admitted for surgery due to hip fractures between 2008 and 2018.
The study analysed data from the 59,943 Taiwanese patients living with osteoporosis who were admitted for hip fracture surgery during the specified timeframe. Among these patients, 22,494 (37.5 per cent) had received anti-osteoporotic treatment, while 37,449 (62.5 per cent) had not been prescribed any treatment for osteoporosis. Anti-osteoporotic treatments recognised in the study included alendronate, risedronate, ibandronate, zoledronic acid, denosumab, raloxifene, bazedoxifene, and teriparatide (noting patients who were prescribed these medications for anti-cancer purposes were excluded from the analysis).
Results from the study revealed anti-osteoporosis treatment was associated with a 31 per cent reduction in all-cause mortality after hip fracture. Furthermore, patients who received anti-osteoporotic medication for more than one, two and three years, exhibited proportional reductions in all-cause mortality, indicating that those who receive medication for longer periods of time may have a lower risk of mortality.
Significantly, the results revealed that mortality risk was reduced by 71 per cent in patients who had used medication for three years or more. However, in recognition that short-term mortality may have no correlation with whether the patient used anti-osteoporotic medication or not, the researchers excluded the data of 20,759 patients who died within two years of experiencing a hip fracture. Following this additional analysis, it was found that mortality risk was reduced by 54 per cent in patients who had used medication for more than three years.
According to Vice-Superintendent and Executive Director of the National Taiwan University Hsin-Chu Hospital , and Co-Chair of the APFFA Joint Steering Committee, Professor Derrick Chan, Taiwan, improving the quality of care of patients post- hip fracture is crucial, in order to reduce the mortality rate, and risk of re-fracture.
“In response to Taiwan’s rapidly ageing society, and the high incidence of osteoporotic hip fractures, it is imperative that osteoporosis treatment following a hip fracture is initiated.
“In addition, the provision of fracture liaison services (FLS) have been shown to improve osteoporosis-related fracture outcomes, leading to significant increases in bone mineral density (BMD) testing, treatment initiation, adherence to treatment, and a reduction in re-fracture incidence and mortality,” said Prof Chan.
To read the report, click here.