Three leading international organisations have joined forces to develop key performance indicators (KPIs) designed to guide quality improvement in Fracture Liaison Services (FLSs), in response to the nine million fragility fractures occurring worldwide each year that are weighing heavily on healthcare systems.
A recent paper published in Osteoporosis International outlines collaborative strategies formulated by the International Osteoporosis Foundation (IOF), Fragility Fracture Network (FFN) and National Osteoporosis Foundation (NOF) to measure the effectiveness of FLS performance at a patient level.
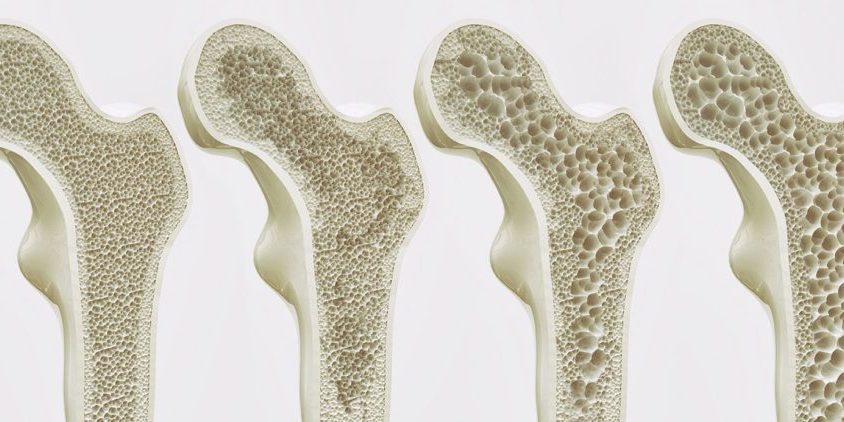
Global prioritisation of osteoporosis, a chronic and often devastating disease, has driven international societies to advocate for worldwide implementation of FLS – a coordinated, multi-disciplinary approach that strives to ensure all patients aged 50 years or above who present to services with a fragility fracture, undergo a risk assessment and receive appropriate treatment and follow-up.
FLS programs have been shown to improve osteoporosis-related fracture outcomes, with significant increases in bone mineral density (BMD) testing, treatment initiation, adherence to treatment and a reduction in re-fracture incidence and mortality.
The IOFs Capture the Fracture Best Practice Framework (BPF) assesses FLS at the organisational level. Thirteen standards measure the scope of the FLS, which has been implemented globally across 380 sites.
According to Prof. Cyrus Cooper, President of the IOF and Professor of Musculoskeletal Science at the University of Oxford, in order to maximise FLS capabilities for optimal secondary fracture prevention within the context of local challenges and opportunities, a set of 11 complementary KPIs within the constructs of ‘a plan-do-study-act methodology’, have been developed.
“The BPF is a globally recognised guidance which has been widely implemented to assess the organisational components of an FLS. For established FLS, the new patient-level KPI set represents an important second step, providing a valuable new tool to examine their current performance at the patient level, and to identify specific aspects of their routine service provision which can be improved. It will also permit further benchmarking against FLSs regionally, nationally and internationally.”
The recommended KPIs can be utilised as tools to improve service delivery with existing resources, and as a means to describe to payers and funders, the precise service gaps present when commissioning and monitoring FLS.
Indicators
Indicator 1: Identification of patients with non-spine fragility fractures:
Identifying all patients with a non-spine fragility fracture is the first step for a FLS. This reflects the number of patients identified by the FLS.
Indicator 2: Identification of patients with spine fractures
A separate indicator for spinal fractures is included, given spinal fractures are both a common and powerful predictor of imminent fracture risk, and noting the care pathway for identifying spine fractures differs significantly from other fractures.
Indicator 3: Initial investigation, including fracture risk assessment within 12 weeks
An appreciation of the imminent fracture risk following the incidence of a sentinel fracture requires rapid assessment, and should ideally be part of the initial management system.
Indicator 4: DXA within 12 weeks
DXA (a bone density test) can be used to classify patients into high vs. low risk of subsequent fracture, as well as a baseline measure for future comparative measurements.
Indicator 5: Falls risk assessment
Reflects the number of patients who have undergone a falls assessment or screening, and those recommended, referred to, or already under a falls service.
Indicator 6: Anti-osteoporosis medication (AOM) recommended as appropriate
Ensuring enough high-risk patients are recommended AOM is integral to reducing secondary fractures at the population level. Given most FLSs are delivered by nurses or allied healthcare professionals with limited prescribing authority, this indicator accounts for patients who are referred to a clinician for AOM recommendation.
Indicator 7: Recorded follow-up within 16 weeks post-index fracture
Given the heightened potential for re-fracture, it is important patients receive timely follow-up to ensure adherence to anti-osteoporosis treatment recommendations.
Indicator 8: Commenced AOM by 16 weeks post index fracture
AOM use reduces fracture risk by 20–86 per cent. This indicator reflects the number of patients who have commenced, or are continuing AOM within 16 weeks of the date of fracture.
Indicator 9: Strength and balance commenced within 16 weeks of fracture
Reflects the number of patients initiating an evidenced-based strength and balance class within 16 weeks of the date of fracture, in accordance with regional or national guidelines.
Indicator 10: Patients taking AOM 52 weeks after the sentinel fracture
In the real-world setting, recorded persistence of anti-osteoporosis treatment for FLS is sub-optimal, and therefore, remains integral to a FLS. Adherence to long-term oral and injectable therapies is vital for a FLS to be effective.
Indicator 11: Data completeness
This indicator measures how many of the preceding indicators have, at minimum, 80 per cent of data completion.
To effectively utilise these metrics and guide quality improvement in FLS, additional time, resources and training of FLS practitioners is necessary.
“Since the introduction of the IOF’s Capture the Fracture Program, there have been many new FLS services established in the Asia Pacific region. Besides using the Best Practice Framework, many FLS services are mapped successfully in the IOF Capture the Fracture Map,” said Dato’ Dr. Joon-Kiong Lee, Department Head of Orthopaedic Surgery and Consultant Orthopaedic Surgeon, Beacon Hospital, Malaysia.
“In order to improve patient care after fragility fractures, both national and regional organisations, including APFFA, should collaborate with IOF to promote FLS services, to provide the best possible care for our patients. We should be aligned in our vision and mission to bring our post fracture patients closer to our heart.”
To stay up to date with APFFA’s progress in driving policy change, improving awareness of, and changing mindsets to optimise fragility fracture management in Asia Pacific, follow us on LinkedIn.