Vertebral fragility fractures (VFFs) are the most common type of osteoporotic fracture and are commonly associated with severe pain, disability and a decline in quality of life, mobility and social participation. The incidence of VFFs increases with age, occurring in 12 per cent of women aged 50 – 79 years, and in 20 per cent of women aged over 80 years.
Although common and frequently present on imaging, VFFs are rarely reported. To address this, in June 2021, The Royal College of Radiologists published a new Radiological guidance for the recognition and reporting of osteoporotic vertebral fragility fractures (VFFs) designed to facilitate radiological recognition and actionable reporting of osteoporotic VFFs.
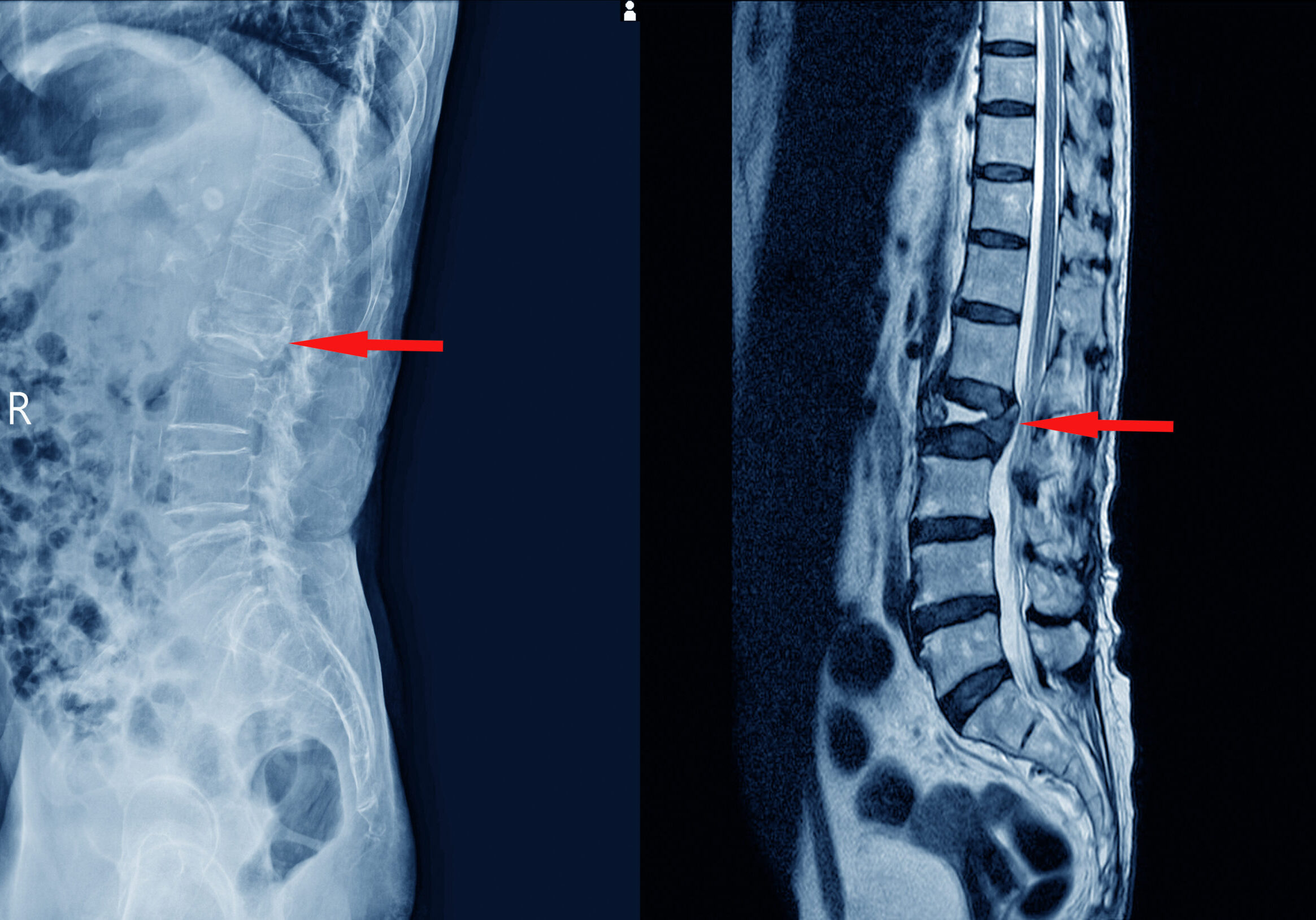
The Guidance was developed following findings from a UK-wide audit performed by The Royal College of Radiologists in 2019. The audit evaluated the organisational reporting infrastructure and specific patient-related reporting data in the diagnosis of VFFs on computerised tomography (CT) scans, in particular where the thoraco-lumbar spine was included in the field of view, but was not the area of clinical interest.
The audit revealed the failure of radiologists to consistently review spinal components on imaging, report on bone integrity and severity of fractures, use correct reporting terminology, and provide adequate onward referral systems, such as fracture liaison services (FLS) or the equivalent.
The Guidance provides the following 12 key recommendations for radiologists and radiographers to move towards a more uniform way of identifying and reporting fractures in daily practise:
- If possible, appoint a radiology osteoporosis lead to support the development, delivery and audit of policy and protocol in the identification and reporting of fragility fractures (including VFFS), and to act as part of a multidisciplinary team (within a local FLS if available).
- Agree on local policies for the opportunistic reporting of VFFs from imaging that includes the spine.
- Agree on local policies for adopting a consistent approach to the identification and reporting of VFFs.
- Implement a policy of automatic sagittal spinal reformatting, display and storage on picture archiving and communication systems (PACS) for cross-sectional imaging studies that include the spine.
- Consider a policy for template reporting of cross-sectional imaging studies that include the spine to include bone integrity, presence of VFF, level and grade/severity.
- Implement a policy for standardised use of terminology for VFFs, using the term, ‘vertebral fracture’.
- Implement routine audit processes around identification and reporting of VFFs.
- Agree on a local policy for onward alerting of referrers or referral to fracture prevention pathways.
- Agree on service level agreements (SLA) with teleradiology contractors to adopt and adhere to VFF-reporting policies.
- Consider the use of standard phrases or short codes to create actionable reports or alerts to referrers.
- Where artificial intelligence (AI) technology is implemented to actively screen cross-sectional imaging, agree processes and policy for radiological correlation and alert reporting.
- Discuss and agree the use of alerts, report content and automisation, and clarify onward referral pathways. Severe or multiple VFFs or cases with canal compromise (ratio of the canal area of the injured level to the average of that of the two adjacent uninjured segments) will warrant urgent clinical evaluation.
The new Guidance has been endorsed by the British Society of Skeletal Radiologists, the Royal College of Physicians and the Royal Osteoporosis Society. It is applicable to all individuals who report imaging that may incorporate the spine, including radiologists reporting onsite and offsite (including teleradiology), and reporting radiographers.
The Guidance offers radiologists and radiographers the opportunity to make a significant positive impact on the health and wellbeing of patients living with osteoporosis and VFFs, and reinforces the importance of accurate and timely reporting of VFFs.
For more information, and to download the full Guidance, click here.
To gain access to many more informative resources, in addition to The Royal College of Radiologists guidance, please visit the APFFA Education Directory at apfracturealliance.org/education-directory.