According to a new review, a significant proportion of the systematic approach to care and prevention of fragility fractures proposed in Osteoporosis New Zealand’s BoneCare 2020 was developed and implemented during 2012 to 2022. However, progression of existing initiatives, and the introduction of new initiatives are required to further address fracture prevention in the country.
The review, titled Experience of a systematic approach to care and prevention of fragility fractures in New Zealand, just published in the journal Archives of Osteoporosis, describes the development and implementation of a systematic approach to both care and prevention for New Zealanders living with fragility fractures, and those at high risk of first fracture.
In 2012, Osteoporosis New Zealand published BoneCare 2020: A systematic approach to hip fracture care and prevention for New Zealand. At the time of publication, New Zealand lacked a coordinated, national strategy and systems to optimally manage those who sustained fragility fractures. This systematic approach to bone health in New Zealand successfully engaged a broad array of stakeholders to work towards mutually agreed goals.
An informal alliance of organisations progressed implementation of the objectives proposed in BoneCare 2020 during 2012 to 2016. However, the alliance was formalised in 2017, under the Live Stronger for Longer programme. Partners and contributors include the Accident Compensation Corporation (ACC), Ministry of Health, Health Quality and Safety Commission New Zealand, Osteoporosis New Zealand, Carers New Zealand, Age Concern, St. John Ambulance, Stroke Foundation of New Zealand, District Health Boards, Primary Health Organisations, and representatives of healthcare professional organisations.
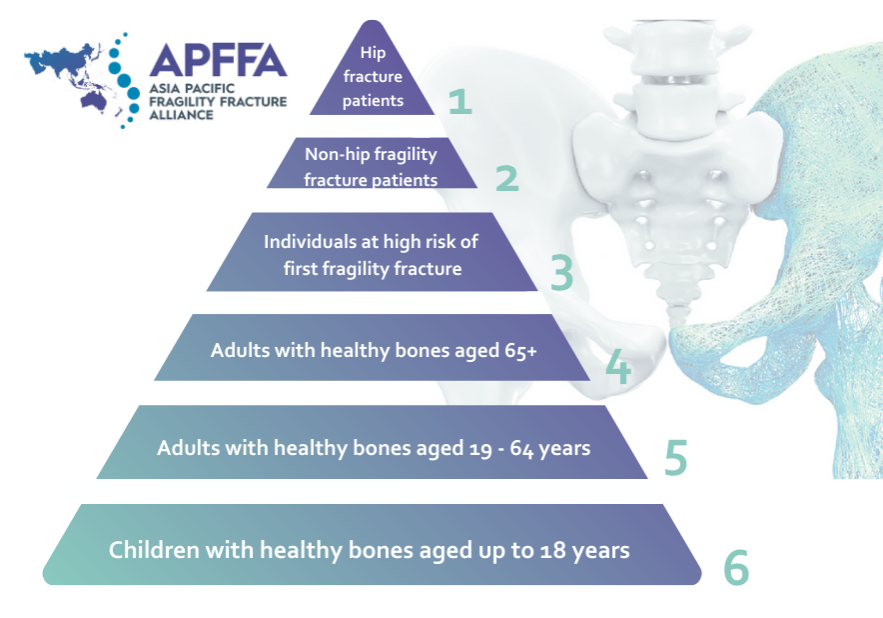
The authors reviewed how each of the following six objectives outlined in BoneCare 2020 were implemented across New Zealand throughout 2012 to 2022:
- Improve outcomes and quality of care after hip fractures by delivering Australian and New Zealand professional standards of care monitored by the New Zealand Hip Fracture Registry.
- Respond to the first fracture, to prevent the second, through universal access to Fracture Liaison Services (FLS) in every District Health Board in New Zealand.
- General practitioners (GPs) to stratify fracture risk within their practice population utilising fracture risk assessment tools supported by local access to axial bone densitometry.
- Consistent delivery of public health messages – to adults with healthy bones aged 65 years and over – on preserving physical activity, healthy lifestyles and reducing environmental hazards.
- Consistent delivery of public health messages – to adults with healthy bones aged 19–64 years – to exercise regularly, eat well to maintain a healthy body weight, and create healthy lifestyle habits.
- Consistent delivery of public health messages – to children with healthy bones aged up to 18 years – on accrual of peak bone mass through a well-balanced diet and regular exercise, which promotes bone development.
The authors note the majority of the progress made in implementing the systematic approach to care and prevention of fragility fractures proposed in Osteoporosis New Zealand’s BoneCare 2020, has been facilitated by a national alliance of stakeholder organisations from different sectors. This has primarily been in relation to the care of individuals who have sustained hip, or other fragility fractures, supported by the production of clinical standards and registries to benchmark the provision of care. The creation of a consumer-facing, not-for-profit “brand” emphasising bone health, rather than osteoporosis, is showing early promise in the promotion of greater public awareness.
The authors proposed the progression of existing initiatives and the introduction of new initiatives for 2022 to 2030. According to the six objectives proposed in BoneCare 2020, achievements by 2030 should include:
Objective 1: The care of people who sustain hip fractures to be documented in the New Zealand arm of the Australian and New Zealand Hip Fracture Registry, and, from 2023 to 2030, all patients to receive best practice as described by the Australian and New Zealand Hip Fracture Care Clinical Care Standard.
Objective 2: Universal access to IOF-accredited Gold Star FLS to be available from 2025, and for the care of those who sustain fragility fractures at any relevant skeletal site, to be benchmarked against the second edition of the Clinical Standards for FLS in New Zealand, in the New Zealand arm of the Australian and New Zealand Fragility Fracture Registry.
Objective 3: A collaboration led by the Royal New Zealand College of General Practitioners, Osteoporosis New Zealand, Ministry of Health, Health NZ, Māori Health Authority, and ACC, to ensure reliable identification, investigation, and interventions for all New Zealanders who are at high risk of sustaining fragility fractures, underpinned by state-of-the-art information technology solutions and regularly updated national clinical guidance.
Objective 4: New Zealanders aged 65 years or over to complete the Know your Bones™ online self-assessment, and discuss their personalised report with their GP. Osteoporosis New Zealand, ACC, and the Ministry of Health to collaborate to develop awareness campaigns relating to preserving physical activity, healthy lifestyles, and reducing environmental hazards.
Objective 5: New Zealanders aged 50–64 years to complete the Know your Bones™ online self-assessment, and discuss their personalised report with their GP. Osteoporosis New Zealand to collaborate with all relevant stakeholder organisations to develop awareness campaigns relating to regular exercise, nutrition to maintain a healthy body weight, and creating healthy lifestyle habits.
Objective 6: Osteoporosis New Zealand to collaborate with the Ministry of Education, academic educators, and teachers, and their professional organisations, to incorporate content relating to bone health into the school curricula for science, health and physical education.
Osteoporosis New Zealand is committed to collaboratively developing BoneCare 2030 with all organisations that have contributed to date, and to expand the stakeholder group to strengthen the approach for aspects where limited progress has been made, including the consideration of equitable outcomes being actively designed for, and monitored.
To read the full article, click here.