With the publication of the United Nation’s 2017 report on World Population Prospects illustrating the impending demographic shift the world was set to experience, clinical leaders were motivated into recognising and acting on the challenges associated with the rapidly ageing global population.
It has become glaringly obvious that older people will need to remain independent for much longer, with fracture prevention and optimal restoration of function post- fracture an absolute necessity.
An overview of the multidisciplinary approach to fragility fractures around the world is available in the recently published second edition of Orthogeriatrics – The Management of Older Patients with Fragility Fractures. The ‘orthogeriatric approach’ to fragility fractures referred to in this text, describes the entire post-fracture pathway, including rehabilitation and secondary prevention, as well as multidisciplinary co-management of the acute fracture episode.
The Global Call to Action, the biproduct of collaborative efforts involving the Fragility Fracture Network (FFN) and five other international organisations* designed to tackle the burden of fragility fractures, has been accounted for in this revised edition.
The recommendations established through the Global Call to Action can be summarised by the following four pillars:
- Multidisciplinary care of the acute fracture episode with an orthogeriatric approach.
- Excellent rehabilitation to recover function, independence and quality of life, commencing immediately after injury, but continued long-term.
- Reliable secondary prevention after every fragility fracture, addressing falls risk and bone health.
- Formation of multidisciplinary national alliances to promote policy change enabling the above-mentioned three pillars.
This text emphasises the principles within each pillar, and where applicable, provides a list of essential practical steps towards implementation. The establishment of national Fragility Fracture Networks (FFNs) is proposed as a catalyst to drive establishment of the national alliances of healthcare professional organisations advocated in the fourth pillar.
The various sections of this all-inclusive text covers:
Background information
The book offers comprehensive insights and background information on the epidemiology of fractures and social costs. Several chapters delve into the critical risk factors for fracture, including age, the incidence of previous fracture, and a family history of hip fractures.
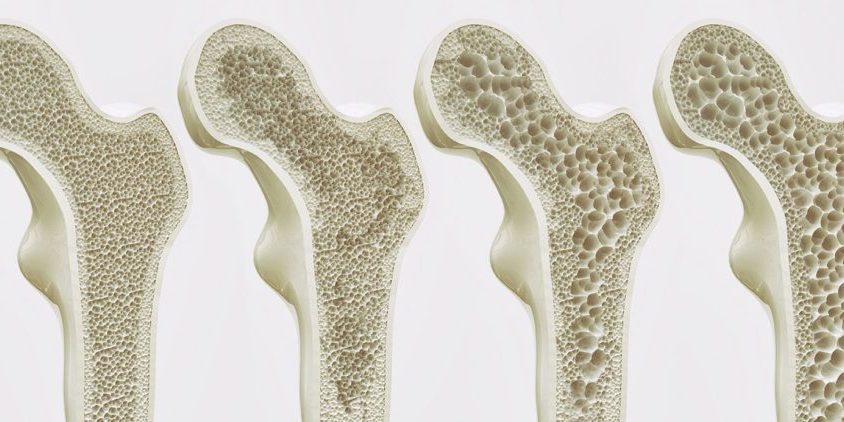
Patients who present with fragility fractures are experiencing two separate issues. The first is bone fragility due to osteoporosis or osteopenia, which has allowed the fracture to occur with minimal trauma. The second is frailtyof their whole body, which compromises their capacity to respond to stress, and is associated with comorbidities. The prominent role of sarcopenia in frailty, analogous to that of osteoporosis in fragility, is explained.
Co-management in the acute episode
Orthopaedic surgeons are proficient at dealing with the fragility, while geriatricians are trained to address frailty. The older patients with fragility fractures, therefore, require the application of both skill sets if they are to emerge from the experience with good health and function. This is the basic argument for the need for orthogeriatric co-management.
Rehabilitation (Pillar II)
One of the implications of the predicted demographic changes over the ensuing few decades is the need for more effective rehabilitation after a fragility fracture, to ensure dependency is minimised. Importantly, as the global population ages, more of the responsibility and care for affected individuals will fall to their family carers, as existing services in all countries become increasingly overwhelmed.
Secondary prevention – Fractures beget fractures
During the first five years after sustaining a fracture, approximately one-in-five patients will sustain a subsequent fracture, with the highest risk occurring during the two years post- initial fracture. In order to satisfactorily prevent further fractures, both the osteoporosis and falls risk must be addressed as soon as possible after the initial fragility fracture has been sustained.
Given currently available treatments almost halve fracture risk, there is the potential to prevent one-in-four subsequent hip fractures.
Unfortunately, a concerning 70-85 per cent of patients currently presenting to their primary care physicians or hospital with a minimal trauma fracture, are neither assessed for osteoporosis, nor appropriately managed to prevent further fractures. This highlights the urgent need for reconfiguration of fracture services to capture every fragility fracture, and to link them to the appropriate bone health and falls prevention services.
The role of nurses
The volume of fragility fracture-related work is such that it cannot realistically be delivered without enhanced nurse input. There will not be (i) enough geriatricians to deliver orthogeriatric surveillance of all older fracture inpatients on a daily basis or (ii) enough endocrinologists for every fragility fracture patient to be assessed for secondary prevention by a doctor. This text explores the key nursing roles and interventions relating to orthogeriatric nursing care.
During the two months since open access publication of the textbook in August 2020, 124,000 downloads of the textbook have occurred. FFN is working to disseminate the book to all healthcare professionals globally with an interest in managing individuals who sustain fragility fractures.
On October 24, 2020, FFN published two toolkits on their website that complement this textbook:
- Clinical Toolkit, concerned with the practical implementation of Pillars I–III; and
- Policy Toolkit, which expands on the fourth pillar of the healthcare policy change and the work of the national FFNs.
The FFN represents one of seven global and regional member organisations from the geriatrics, orthopaedics, osteoporosis and rehabilitation sectors, that constitute our organisation – the Asia Pacific Fragility Fracture Alliance (APFFA), which is committed to improving the acute care, rehabilitation and secondary prevention of fragility fractures throughout the Asia Pacific region.
Our primary purpose at APFFA is to drive policy change, improve awareness of, and change political and professional mindsets to facilitate optimal fragility fracture management. Our mission is to promote multidisciplinary collaboration and change policy to facilitate best practice in the acute care, rehabilitation and secondary prevention of fragility fractures.
*The European Federation of National Associations of Orthopaedics and Traumatology (EFORT), European Union Geriatric Medicine Society (EuGMS), International Collaboration of Orthopaedic Nursing (ICON), International Geriatric Fracture Society (IGFS) and the International Osteoporosis Foundation (IOF).